RCM automated for Behavioral Health.
See how AI Agents recover uncollected revenue, accelerate insurance verification, and streamline patient intake without you lifting a finger.


Unmatched Outcomes
97%
Accuracy on clinical & demographic data
~60%
FTE bandwidth
saved
$500K
Added collections
in 4 months
Faster payment. Stronger compliance. Higher margins

Coordinating Intake
Sarah handles missed calls and new leads instantly. Automates call-backs, appointment booking, and patient hand-offs.





Eligibility & Benefits
Susan checks eligibility before every appointment, flags network status, and projects patient responsibility to prevent revenue roadblocks





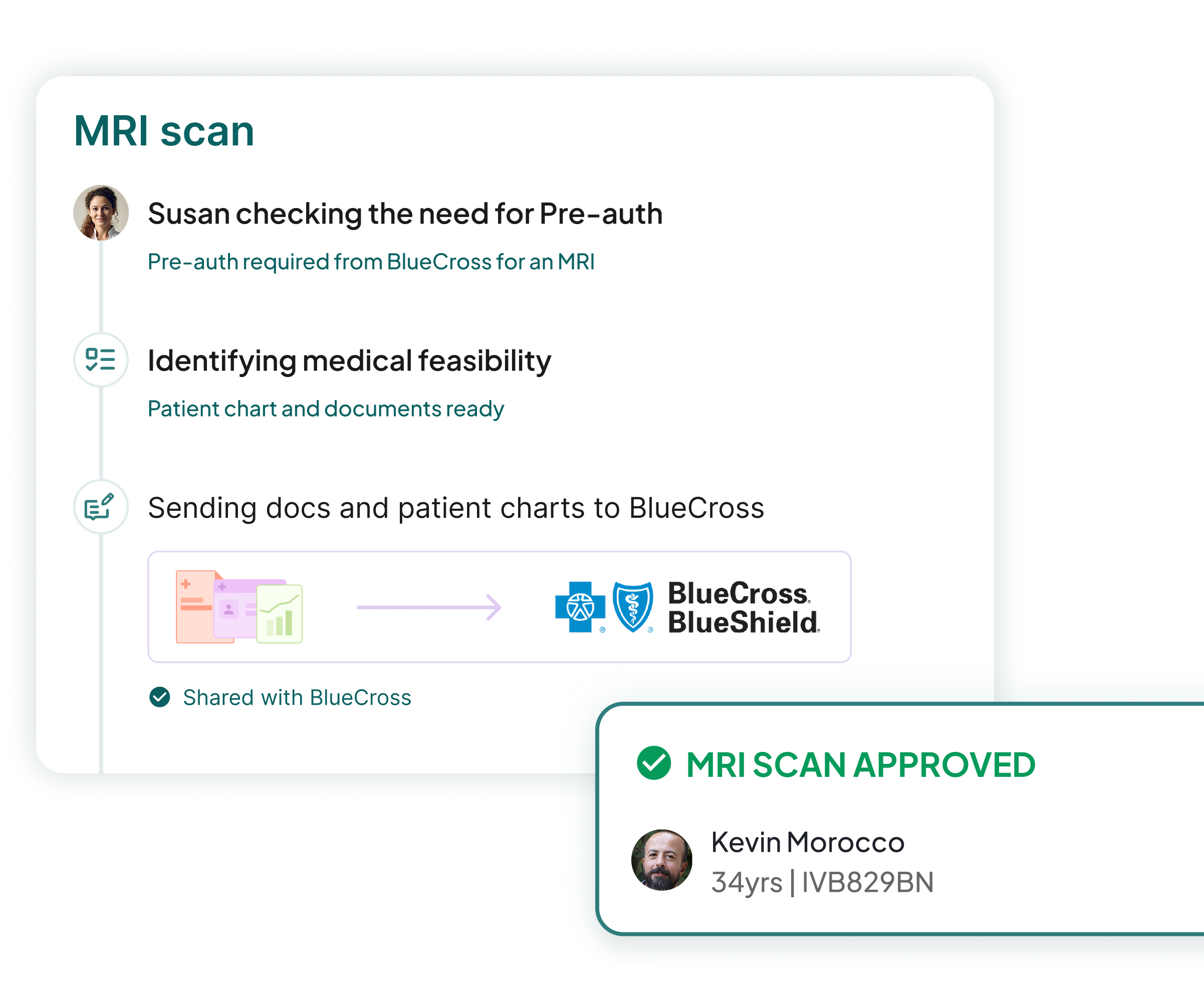
Prior Authorization
Runs benefits checks across 3000+ payers, flags auth needs, and builds packets



Appointment Scheduling
Selena schedules appointments and manages cancellations, fills empty slots, and maximizes appointment capacity with no missed opportunities.





Charge Review
Sage codes and analyzes every claim as soon as visit notes are added in your EHR, and fixes any coding errors - ensuring 95%+ first-pass clean claims.





AR and Payment Posting
Sean monitors charges and EOBs in real time, interprets CARC codes, reconciles payments and write offs, and flags mismatches between approvals and bank deposits to prevent denials.



Workflow for Behavioral Health Practices
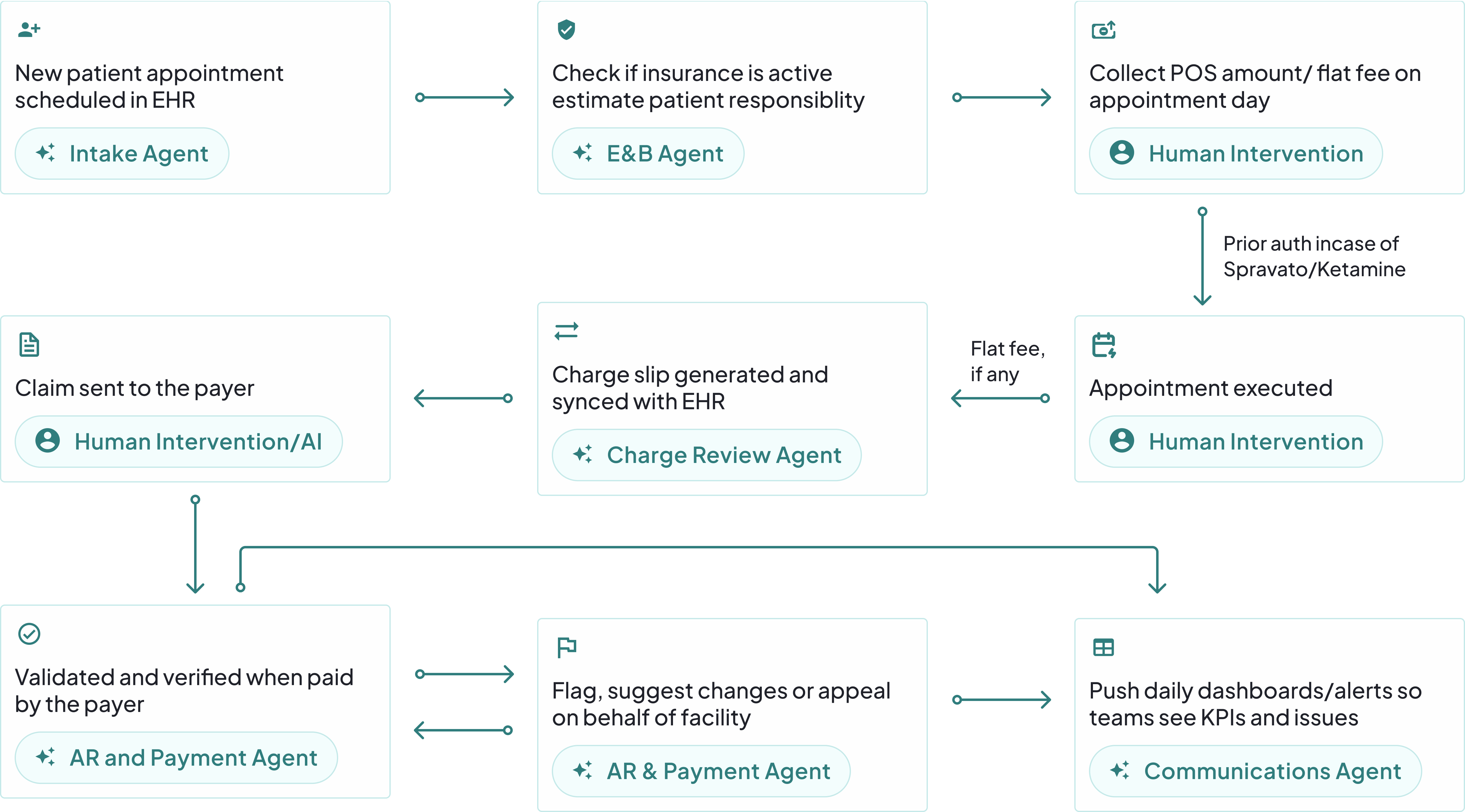

Have a different workflow? Customize it for yourself!
Book a free demo call with our team
True Agentic AI that works in the background, right inside your EHR, CRM & Workplace tools
Tired of managing endless AI software logins? So are we.




















Our AI Agents work on top of your unique workflows, systems & EHRs.
Unmatched productivity
Cut denial rates from ~20% to <5%, boosting revenue.
High-acuity patients enrolled & processed 90% faster

7-day authorizations? Try 24 hours from application to confirmation.
Uncover hidden coverage, recover up to 15% write-offs.
Paperwork gone, reimbursement accelerated.
Lower DSO by 15-20 days, improve cash flow with early visibility.
Maximize revenue, minimize admin. behavioral health practice automated
What makes us so sure?

100 charges
processed every minute
5M + Charges processed this year

230 appeals
made per day
4M + appeals files processed this year

700 man hours
saved every day
5M + Charges processed this year

$100 Million
saved this year
$ 900M + dollars saved
Consult with our Automation Team today!
Why partner with us?
Nanonets Health streamlines revenue cycle management with secure, compliant AI automation.
HIPAA Compliant
Streamlined revenue cycle management with secure, compliant AI automation.
SOC 2 Certified
Verified controls exceed healthcare standards for data protection.
3X ROI Guarantee
ROI documented within 6 months across all specialties.
24/7 AI Automation
Agents run nonstop, eliminating manual tasks and speeding revenue capture.

Evidence-Based Results
Proven outcomes across 300+ healthcare organizations.
Seamless Integration
Works with all EHRs without disrupting workflows or IT.


















.svg)
.svg)
.svg)



