
Automate eligibility verification and prior auth across 1500+ payers

95% reduction in verification time

80% lower processing costs

8x more verification per hour
Unified automation for all payer-facing tasks
Susan, our bespoke AI agent, handles all manual tasks for your insurance discovery and eligibility needs.
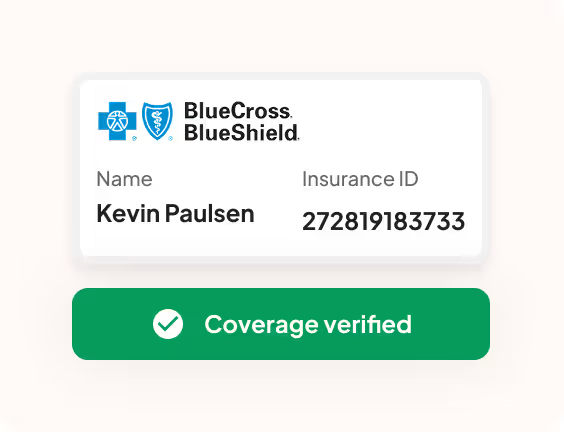
STEP 1
Patient Coverage Check
Susan starts by checking if insurance information is present in the patient's records, including member ID & provider details. If any crucial information is missing, Susan automatically notifies the intake team.
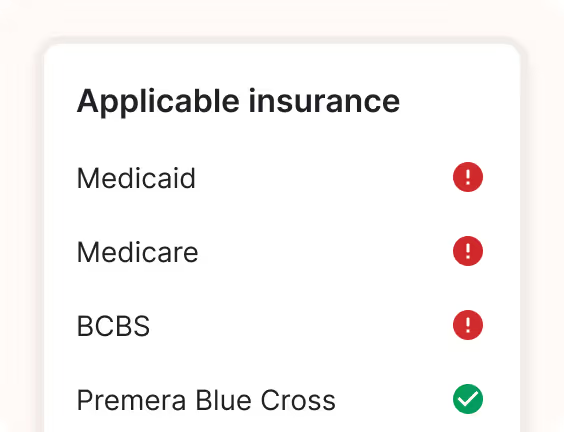
STEP 2
Insurance Discovery
When member ID isn't available, Susan automatically searches across insurance databases to find active coverage. Sam checks multiple sources including Medicare and Medicaid to ensure no coverage is missed.
STEP 3
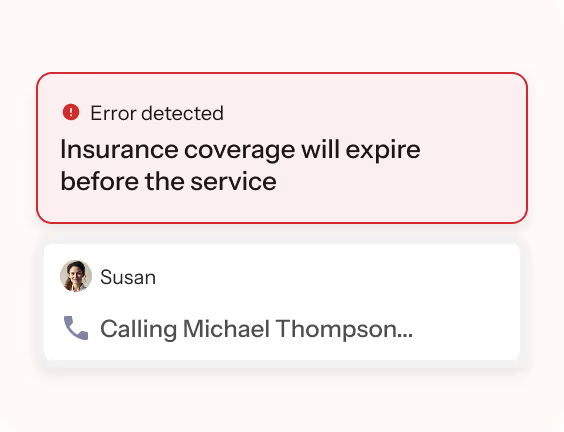
Real-time Eligibility Verification
Susan verifies insurance coverage in real-time, checking if the specific services are covered under the patient's plan. This includes confirming the provider network status and service type coverage.
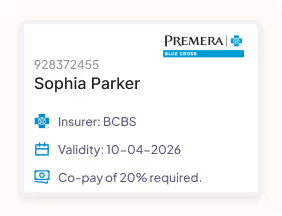
STEP 4
Benefits Summary
Susan generates a comprehensive benefits summary showing copays, deductibles, out-of-pocket maximums, and covered services. If multiple insurance policies are found, Sam flags this for proper coordination of benefits
See the complete list of payers we support
Don't see the payer you want listed below? Get in touch and we'll get them added.
Consult with our automation team today!
Be the change you want to see; speak with our team today.















